Video interview wiht John Lynne (@Techguy and @EHRandHIT) on topics ranging from EHR Upcoding, Meaningful Use Stage 2, Interoperability, EHR Consolidation, and ACOs (originally posted here):
Monday, October 29, 2012
November Voice of the Doctor Guests
An exciting month for Voice of the Doctor with the following guests appearing
November 2: Terri Mitchell, MSN RN
Director, Clinical Informatics Solutions at Nuance Communications
We will be talking about The Healthcare Data Imperative and the challenge of capturing Healthcare data and the importance of capturing information at the point of care when the information is fresh in the mind and the value this brings to affecting a postive change in healthcare quality outcomes and appropriate reimbursement. We will discuss the need to focus on real time vs retrospective analysis and how this can be achieved in our new digital world of electronic medical records and the value of patient engagement as part of this process.
November 9: Dr Ashish Jha, MD
The C. Boyden Gray Associate Professor of Health Policy and Management at the Harvard School of Public Health and blogs at An Ounce of Evidence
He wrote this piece: Asking the Wrong Questions About the Electronic Health Record that was a response to the article posted recently on the Wall Street Journal: A Major Glitch for Digitized Health-Care Records that stated:
Now, a comprehensive evaluation of the scientific literature has confirmed what many researchers suspected: The savings claimed by government agencies and vendors of health IT are little more than hype.
And was subject to many active discussions on several of the listservs. Dr Ashish Jha and I will be discussing some of the fundamental issues of our broken system and the challenges faced in our archaic paper based system which most can agree do nothing to empower clincians to provide excellent care. Technology on its own cannot provide all the answers but must be part of a broader based solution.
The problem is that some Health IT boosters over-hyped EHRs. They argued that simply installing EHRs will transform healthcare, improve quality, save money, solve the national debt crisis, and bring about world peace. We are shocked to discover it hasn’t happened – and it won’t in the current healthcare system.
We need to leverage the potential by asking and answering other related questions
- How do we create incentives in the marketplace that reward physicians who are high quality?
- How do we allow physicians to capture efficiency gains?
- What to do about fee for service - are ACO's the answer?
- How does technology play an effective part in this transformation
As Dr Jha said:
The debate over whether we should have EHRs is over. Can we fix our broken healthcare system without a robust electronic health information infrastructure? We can’t. Instead of re-litigating that, we need to spend the next five years figuring out how to use EHRs to help us solve the big problems in healthcare.
Should be a great discussion
And to close out November I am excited to announce that I will be joined by Dr Eric Topol, MD
November 16, Dr Eric Topol, MD
Professor of Genomics at The Scripps Research Institute
Follow him on twitter @EricTopol
He is also the author ofThe Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care and has named in the list of the Top 100 Most Influential Physician Executive in Healthcare, 2012 by Modern Healthcare
If you have not read the book, you should. You can read the First Chapter here: The Digital Landscape: Cultivating a Data-Driven, Participatory Culture to get a taste for the wide open opportunites many of which are here and even more coming in the very near future. With so many topics to choose from:
- The Current state of medicine and the challenges
- Individualized medicine vs Group Thinking
- Patient Engagement and the power of mobile Health technology
- The Genome and Sequencing (Dr Topol recently had his genome sequenced - one of an expanding number of people to do so):
We've got our genomes sequenced, now zooming in on them bit.ly/OWh6eW @illumina w/ @gholsonlyon @bradpatay
— Eric Topol (@EricTopol) October 22, 2012
And Posted some initial analysis with a 99c App!
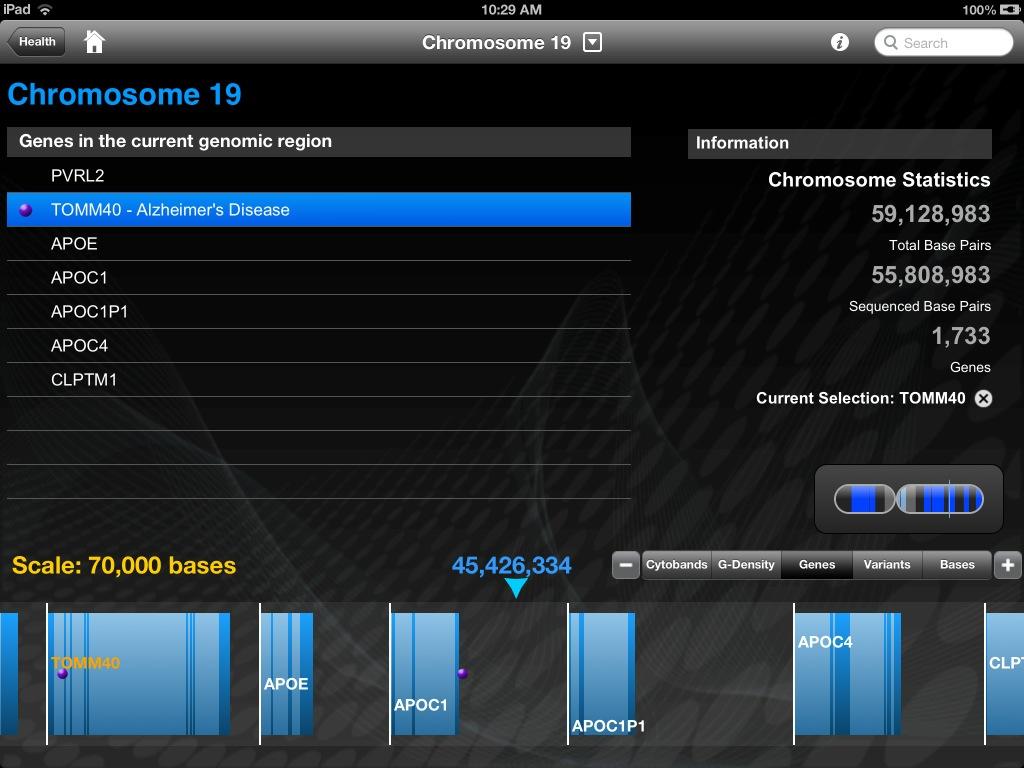
So many topics and so little time. Focusing on the current challenges in Alzheimer's treatment makes much of this come into focus. A recent story on NPR: Treatment For Alzheimer's Should Start Years Before Disease Sets In raises one of the big challenges in this disease....How do we know if we need to commence treatment for a disease. It seems unlikley that any preventative treatment can be given to everyone so identyfying those at risk will become a major focus in the coming years. As Dr Topol noted in his book and in many of his presentations and discussions on the effectiveness of Plavix varies based on presentation of the genotype CYP2C19. This was subject to an extensive debate and included this posting on the Topolog posting An important miscue in clopidogrel pharmacogenomics and in a perfect example of the use of technology and engagement this videoif this works here otherwise download a verion here)
Since November 23 is the day after Thanksgiving we will have a re-run on November 23 and Nov 30 from a previous shows
Hope you can join me
Join me on Friday at 2:30 ET on VoiceoftheDoctor
Adding Voice Recognition To Mobile EHRs
The new world of Mobile Healthcare will include an integral component in efficiency - the power of he clinicians voice. Cerner and Epic are
The new mobile-native electronic health records (EHRs) systems of Epic and Cerner are being voice-enabled via recent deals with Nuance Communications
Not only easy access to the world's leading speech recognition platform but as Joe Petro (SVP for R&D at Nuance) puts it:
it's form-factor neutral and can be used with iOS, Android, or other mobile or desktop devices, as well as thick- and thin-client systems
Great news for the mobile platform making these devices as productive as they can be
Wednesday, October 24, 2012
Will Nuance's Nina Do What Apple's Siri Won't? - Forbes
A series of Forbes Insights profiles of thought leaders changing the business landscape: Gary Clayton, Chief Creative Officer, Nuance
Apple’s Siri iPhone voice-based App interface has forever changed consumer expectations of how to interact with their computing devices. But Nuance’s Nina may represent an even bigger transformation—the consumerization of IT. Nuance has over 10,000 employees, $1.4 billion in revenue in FY ‘11, $7.65 billion market cap company, headquartered in Burlington, Massachusetts and is best known for its Dragon Naturally Speaking voice recognition software. They just might be the biggest, most successful company you never heard of before. They describe themselves as “focused on developing the most human, natural intuitive ways to use your voice to take command of information.”
Siri is cool. But Nina may represent a true leap forward in man-machine learning and artificial intelligence. I recently spoke with Gary Clayton, Nuance’s Chief Creative Officer about his role in bringing Nina to life and his thoughts on how Nina is already bringing a welcome change into how businesses put the tool he helped to create to work to better serve their customers. He’s the guy responsible for turning some of the world’s most sophisticated software algorithms and artificial intelligence into engaging and user-friendly interfaces. He also oversees innovation, strategy and design at Nuance. “I wear a lot of hats,” said the understated Clayton.
The major innovation behind Nina is its capability to retain context over time. People can interact with Nina, the virtual assistant for customer service apps, and carry on a complex set of instructions within the same conversation flow. Its artificial intelligence learns and anticipates the user’s interests and requests over time—using natural language understanding. For example: a person can ask Nina what their checking account balance is, then a person can ask Nina to show them the charges over $200 and then for the month of August, or one could go through the bill paying process by simply stating “I would like to pay the balance on my cable bill on Friday from my savings account.” Humans communicate through context, not through complex, detailed step-by-step instructions that have always been the hallmark of human to computer interaction.
Imagine calling your insurance company and having a pleasant and successful interaction with an always friendly voice. No more yelling and swearing into the phone “Operator”!! Nina can also interact across devices and applications, so that customers can choose to connect by voice, mobile device or web page or any combination and still retain the context of the interaction. In fact, one such enlightened financial services company USAA, is implementing Nina to create a better customer experience. “USAA is extraordinarily responsive to their customers; one of the very best in their field and represent a gold standard in managing the customer experience,” said Clayton.
“People like to anthropomorphize technology,” stated Clayton. He knows it’s a basic human need to understand and control the world around us. Nina is one expression of meeting that need. That’s what drives Clayton in what he calls his never-ending quest to understand the creativity behind science and art. He started his quest as a physics undergrad at SUNY and later ventured to San Francisco for interdisciplinary studies and eventually earned his BA in communication from San Francisco StateUniversity. He sees creativity as the synthesis of art and science.
This led to a fascinating career path that began with the explosion of Silicon Valley technology drawing the film business toNorthern California. There, Francis Ford Coppola, George Lucas and others set up shop. Clayton worked with all of them but most notably Lucas and his Skywalker Ranch studios inMarin County,California, where he engineered sound recordings, which included the first recordings at Skywalker Sound with the San Francisco Ballet Orchestra. He founded and ran his own multi-media production company from 1985 to 2000 and worked on many Academy Award winning films, Grammy winning albums and Emmy winning TV shows. There he worked on projects with Michael Jackson, Dave Brubeck, The Cure, Brian Eno, David Bowie, Mel Torme, Sam Shepard, David Byrne, Norman Mailer, Apple Computer (Knowledge Navigator,Newton) and many others. After a succession of consulting projects at Pacific Bell and a start-up gig at TellMe, (acquired by Microsoft for a reported $800 million in 2007) he spent time at Yahoo where he headed up their speech strategy. From there he landed at Nuance in 2008. Clayton is the owner of eight patents and is considered one of the leaders in the digital speech recognition movement.
As one of the key developers of the Dragon Go! and Nina product lines, he is helping to push Nuance into the forefront of turning mobile device personal assistants into personal advisers. His vision of the synthesis of art and science may be a never-ending process, but his work on Nina just may be the full fruition of a lifetime of trying.
Imagine that - a User friendly EMR interface that uses the power of your voice and a natural exchange to navigate and interact with. The long term memory (or retaining of context) offers a more natural and engaging exchange
The major innovation behind Nina is its capability to retain context over time. People can interact with Nina, the virtual assistant for customer service apps, and carry on a complex set of instructions within the same conversation flow.
The example cited is for your banking exchange but imagine this in healthcare
"Nina show me my patients for today"
"What are the latest laboratory results for Mr Jones"
"Are there any new results on my patients marked abnormal"
You get the picture
Changing the interaction with technology, especially in the mobile world but also in every human/computer interface shielding the user from the complexity of the technology by providing an easy conversational speech front end.
I can hear Scotty now..."a keyboard...how quaint"
Tuesday, October 23, 2012
Doctors Using Electronic Health Records Provide Higher Quality Healthcare | Government Health IT
The use of electronic health records is linked to significantly higher quality care, according to a new study by Lisa Kern and her team, from the Health Information Technology Evaluation Collaborative in the US. Their work appears online in the Journal of General Internal Medicine, published by Springer.
Electronic health records (EHRs) have become a priority in the US, with federal incentives for 'meaningful' use of EHRs. Meaningful use entails tracking and improving specific patient outcomes, as well as gathering and storing information.
Kern and colleagues examined the effect of EHRs on ambulatory care quality in a community-based setting, by comparing the performance of physicians using either EHRs or paper records. They assessed performance on nine specific quality measures for a total of 466 primary care physicians with 74,618 patients, from private practices in the Hudson Valley region of New York.
The quality measures included: eye exams, hemoglobin testing, cholesterol testing, renal function testing for patients with diabetes, colorectal cancer screening, chlamydia screening, breast cancer screening, testing for children with sore throat, and treatment for children with upper respiratory infections.
Approximately half of the physicians studied used EHRs, while the others used paper records. Overall, physicians using EHRs provided higher rates of needed care than physicians using paper, and for four measures in particular: hemoglobin testing in diabetes, breast cancer screening, chlamydia screening, and colorectal cancer screening.
The specific quality measures included in this study are highly relevant to national discussions. Of the seven quality measures expected to be affected by EHRs, all seven are included as clinical quality measures in the federal meaningful use program. There has been little evidence previously that using EHRs actually improves quality for these measures.
This study took place in a community with multiple payers. This is in contrast to integrated delivery systems, such as Kaiser Permanente, Geisinger, and the Veterans Administration, all of which have seen quality improvements with the implementation of health information technology. Most health care is delivered in “open” rather than integrated systems, thus increasing the potential generalizability of this study.
The authors conclude: "We found that EHR use is associated with higher quality ambulatory care in a multi-payer community with concerted efforts to support EHR implementation. In contrast to several recent national and statewide studies, which found no effect of EHR use, this study's finding is consistent with national efforts to promote meaningful use of EHRs."
Brian Ahier works as Health IT Evangelist for Information Systems at Mid-Columbia Medical Center. He is a City Councilor in The Dalles, Oregon and also serves on the Board of Mid-Columbia Council of Government, and Q-Life, an intergovernmental agency providing broadband capacity to the area. He blogs regularly at Healthcare Technology & Government 2.0.
There's been a lot of coverage recently suggesting the Meaningful Use incentive program has failed to deliver value, EHR's have actually induced more cost in healthcare and EHRs have decreased quality of healthcare....
But as Brian Ahier rightly points out there is evidence that supports the value proposition
This study demonstrated value in a typical community setting with multiple players and found real positive impact delivering higher quality care measured by specific measures such as screening and testing for chronic diseases
We found that EHR use is associated with higher quality ambulatory care in a multi-payer community with concerted efforts to support EHR implementation. In contrast to several recent national and statewide studies, which found no effect of EHR use, this study's finding is consistent with national efforts to promote meaningful use of EHRs
Expect more studies that will demonstrate the value
Tuesday, October 16, 2012
The Terrifying State of "Unaccountable" Healthcare
The latest book exposing the healthcare system and how broken it is from Dr Makary a surgeon from Johns Hopkins. As he says
Meet 'Shrek,' a doctor who insists on surgery in every case—and has a surgical-incision infection rate of 20%.
and more troubling
He quotes a recent Hopkins survey of employees of 60 high-quality hospitals, where more than half of the respondents said they would not feel comfortable receiving care in the unit in which they work
He makes the case for flat rate payment that removes the incentive for steering care to individual specialties devoid of any decision making that is for the benefit of the patient.
Take pancreatic cancer, half of Dr. Makary's practice at Hopkins. With only a 15% cure rate, surgery is the only hope. But if the cancer is inoperable, patients may be offered chemo and radiation, which confer minimal benefit and yet make money for doctors and hospitals
There are detractors to this and without incentive there is a corresponding decline in efficiency so finding a balance between these two competing ideals seems necessary
Looks like another book to add to the reading list
Thursday, October 11, 2012
The Health Care Revolution Must be Clinician Centered
The New Yorker author, surgeon, Harvard University faculty member, and health policy adviser Atul Gawande told the President's Council of Advisors on Science and Technology (PCAST) today that checklists could help improve the quality of health care and lower costs. PCAST members seemed enamored with the idea of standardizing treatment and procedures, and also discussed how to raise the academic status of those working in the field. But another PCAST member—Google CEO Eric Schmidt—saw what Gawande was peddling as a potentially lucrative new market for the search engine giant.
Here's Schmidt's dream of what a visit to the doctor will look like in 2015. It came during a question-and-answer session following Gawande's 15-minute presentation, drawn from his new book, The Checklist Manifesto: How to Get Things Right. You can judge for yourself whether it's sensible or scary.
Live Chat: New Therapies for Mental Illness Thursday 3 p.m. EDT"My question has to do with the model of health care that we'll be facing in 5 or 10 years," Schmidt began. "It's pretty clear that we'll have personalized health records, and we'll have the equivalent of a UPC sticker with your medical history. So when you show up at the doctor with some set of symptoms, in my ideal world what would happen is that the doctor would type in the symptoms he or she also observes, and it would be matched against the data in this repository. Then this knowledge engine would use best practices, and all the knowledge in the world to give physicians some sort of standardized guidance. This is a generalized form of the checklists that you're talking about."
Then Schmidt made clear what was troubling him. "As computer scientists, this is a platform database problem, and we do these very, very well, as a general rule. And it befuddles me why medicine hasn't organized itself around these platform opportunities."
Gawande took a shot at responding to the billionaire's bewilderment. "I think part of the bafflement occurs because the folks who know how to make such systems don't understand how the clinical encounter actually operates." But the bigger problem, he said, is that such a search would in all likelihood generate more heat than light for the harried physician, who typically has "15 minutes to manage six problems." According to Gawande, "the three inches of guidance, explaining what the evidence suggests and so on, needs to be turned into a useful form that tells you what you can do."
But Gawande is no Luddite. He told Schmidt that he'd welcome an app—"for your iPhone or whatever the new Google one is"—that could help him the next time he sees a patient diagnosed with a rare renal tumor.
Gawande found a receptive audience for his idea that the federal government create a National Institute of Health Systems Innovation to complement the work of the National Institutes of Health, although PCAST members suggested that he consider other administrative solutions. And they also shared his unhappiness with the relatively low status of health systems analysis. "My sense is that we don't respect this stuff," said PCAST co-chair Eric Lander. "We respect the cancer genome, but not checklists. What do we need to do to send a signal to the next generation of researchers that this is a high-class, worthy thing to do? What would it take to move the needle?"
"You're absolutely right," Gawande replied. "It's not well respected. There's a reason, after all, that I'm still an associate professor."
Older piece from 2012 but an interesting point made by the ever insightful and eloquent @Atul_Gawande when challenged by a non-clincinas who was "Troubled" by the state of #HealthIT.
As Dr Gawande said
I think part of the bafflement occurs because the folks who know how to make such systems don't understand how the clinical encounter actually operates
There you have it - it is easy to look in to healthcare technology and prescribe solutions based on your experience of finance, computers, C++ coding and any other discipline. But if you don't understand the fundamentals of clinical care, the taking of a history and all the nuances involved in teasing out details from patients you can't prescribe a solution that will work effectively
And in a notable humbling point Dr Gawande points out that even within the fences there is resistance to much of the application fo this technology
You're absolutely right...It's not well respected. There's a reason, after all, that I'm still an associate professor
Tuesday, October 9, 2012
The Impact of RACs on Your Medical Practice - Physicians Practice
Please sit down — this will not be an easy article to digest, no matter how carefully I parse my words. Life under the microscope of Recovery Audit Contractors is going to get tougher for physicians. Three recent developments may impact your practice in the next year.
I have written in the past on RACs and documented their growth from a twinkle in Uncle Sam's eye to the behemoths they have become. Much of the advice offered in prior articles (please see links at the bottom of this article) remains valid and should be heeded.
Audits of Level 5 E&M services
CMS has given approval to Connelly, the Region C RAC, to perform complex medical reviews on level 5, E&M services (e.g., 99215, 99205, and 99255). This is the first time CMS has given any RAC permission to target the coding and documentation of E&M services. One impetus for the focus on level 5 E&M services is a shift in providers' use of level 4 and 5 codes. According to the Center for Public Integrity, the percentage of Medicare services coded as level 4 or level 5 increased from 25 percent to 40 percent between 2001 and 2010. This, of course, has increased CMS's financial outlay for these services and made them a much larger budget item (i.e., target).
Connelly is the RAC for thirteen states: Alabama, Arkansas, Colorado, Florida, Georgia, Louisiana, Mississippi, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. Take note: the other three RACs are expected to follow suit.
Since early 2009, the Medical Group Management Association, AMA, and 101 state and specialty societies have actively opposed RAC audits. It is unfortunate for all of us that CMS has not heeded their advice.
There is yet another cause for concern with this initiative. Though it has not been officially confirmed, CMS apparently has given Connelly permission to extrapolate the results of their E&M audits. For instance, if a RAC audit determined that six of twenty (30 percent) level 5 services did not meet coding/documentation guidelines, the RAC would have authority to extrapolate this 30 percent failure rate across all level 5 services provided during the review period.
If you provide level 5 services, it is prudent to have several of them copiously reviewed by a certified professional coder.
9th Circuit Court of Appeals verdict
On September 11, 2012, the U.S. Court of Appeals for the Ninth Circuit rendered a dangerous opinion. It affirmed that RACs are not restricted by regulatory deadlines, statutes of limitations, or time limits. Lead plaintiff attorney Ronald S. Connelly, of Power Pyles Sutter & Verville PC, says "The decision leaves providers with absolutely no finality in their payments from the Medicare program. Contractors could reopen claims that are even 10 or 20 years old, and providers would have no right to challenge the timeliness of the audit."
Legal minds will weigh in on this opinion in the weeks and months to follow, but again, a scary precedent has been set. It may mean that Medicare patient and billing records should be maintained indefinitely. At a minimum, it means the past is neither safe nor sacred.
I recommend you contact your medical malpractice insurance carrier to determine if this circuit court opinion will change their recommendations for records retention.
EHR automated notes
Last but not least, the HHS's Office of Inspector General has set its focus on whether providers are using automated note generation appropriately in their EHRs. Also known as "cloned notes," automated notes and templates use copied and pasted data on multiple patients to record standard information such as a normal review of systems or physical exam.
An observer reviewing several such notes would find virtually identical documentation and very little patient-specific information. Herein lies the OIG's concern. They are concerned that cloned notes may lead to over-documentation or a lack of patient-specific information. From a medical malpractice liability perspective, the same concerns apply.
There is a place for structured notes, and many physicians used them prior to the advent of EHRs. These are acceptable, and EHR-generated notes that contain patient specific documentation should be good to go as well. Your risk lies in over-cloning identical text in your patient notes.
In summary
The United States Department of Justice (DOJ) has three top priorities:
• Terrorism
• Violent crimes
• Healthcare fraudI wish healthcare fraud were not on this list, but it is, and it is not dropping off the list anytime soon. Government oversight and second-guessing are givens for anyone who practices medicine today; expect fraud identification and enforcement initiatives to grow.
To get a head start on audit-proofing your practice, read the following articles that offer advice and practical tips for protecting both yourself and your practice:
• Avoid Medicare Fraud Claims by Coding Correctly
• Medicare's Fraud and Abuse Program
• Nine Things to Know About RACs
Lucien W. Roberts, III, MHA, FACMPE, is vice president of Pulse Systems, Inc., and a former practice administrator. For the past 20 years, he has worked in and consulted with physician practices in areas such as compliance, physician compensation, negotiations, strategic planning, and billing/collections. He can be reached at lroberts@pulseinc.com.
As the article says - "please sit down, this will not be easy"
As they used to say "up north" in England: "there's trouble at Mill" and aptly captured in the Monty Python Sketch ""The Spanish Inquisition"
The recent decision in the 9th circuit court:
affirmed that RACs are not restricted by regulatory deadlines, statutes of limitations, or time limits
and
..the HHS's Office of Inspector General has set its focus on whether providers are using automated note generation appropriately in their EHRs...They are concerned that cloned notes may lead to over-documentation or a lack of patient-specific information. From a medical malpractice liability perspective, the same concerns apply.
It will be important to provide a balance of information derived form templates and structured content supplemented with narrative generated efficiently and not just stored as narrative but understood to be included in the structured information essential to managing patients
Thursday, October 4, 2012
Accelerating Electronic Information Sharing to Improve Quality and Reduce Costs in Health Care
If we are to get better health at lower cost - how can we not engage the patientThe impact of patient engagement in Patient Health - it would be a Blockbuster drug!Providers need to stimulate this activity - since patients are the "Best Fact Checkers in the world"