HIMSS is finally upon us and like the 20,000+ people heading Chicago there is a lot to take in, many options and far too much for any one person to see or catch up with. So what do you do?
First off - download the HIMSS Mobile APP that now comes with GPS intelligence which hopefully will start to provide keen insights into activities and opportunities that are nearby as you move around Chicago, the convention center and beyond
Download and print (I know not very environmentally friendly but there is a lot to absorb) the HIMSS Conference Guide (72 Pages) - or if you are feeling really clever send it to you iDevice, Pocket, Kindle or some other reading device
Or use the online version of the HIMSS of the guide - here
For the physician centric guide - head on over to this living breathing dynamic Google Document - put together by Wen Dombrowski (@HealthcareWen)
For the HIT Centric Guide from John Lynn (@TechGuy)
For the latest and greatest news be sure to follow the #HIMSS15 hashtag, and others linked to the conference including #DrHIT
And your best option for keeping up with the latest and greatest from Symplur tracking system on #HIMSS15 and that page features additional topics and tags worth following and tracking
And of course follow your Social Media (#SoMe) Ambassadors can all be found in this list on twitter
Showing posts with label #healthit. Show all posts
Showing posts with label #healthit. Show all posts
Friday, April 10, 2015
Tuesday, March 24, 2015
Digital Health Technology Trends from SXSW
Great graphic that HITConsultant posted in this update SXSW Health Tech Trends
Health and fitness apps, smart devices and connected products are making us more aware of our own health—and more active participants in our efforts to stay healthy. At the same time, health providers are looking to technology for smarter ways to deliver quality care, whether we are in the hospital or at home.
- Wearable technology - 80% of consumers would benefit from the use of wearable technology
- Connected devices - Using remote monitoring to reduces readmissions
- EHRs - 71% of physicians now use EHRs and 85% meeting current meaningful standards
- Telehealth 70% patients comfortable communicating with their doctor using digital technology vs hauling themselves in to the officer
- Predictive analytics - More than 80% of standard tasks (BP, glucose etc) and even complex testing (e.g. genomics) will change the way we deliver care as described by Eric Topol in "The Patient Will See You Now"
- Population health management - 70% of providers reporting patient care benefits from population health initiatives
- mHealth apps - 71% of want providers to use mobile apps not least of because they do...going where everyone else is
- Data security - rightly ranked as a major issue among consumers given the ongoing debacle of healthcare related security breaches (Premera and Anthem Blue Cross, the HHS wall of shame)
- Partnerships - increasing healthcare companies entering new healthcare partnership - Tenet seem to be the latest
- Cloud-based technology - importantly seen in conjunction with "Data Security" expect this to grow at a staggering 20% rate and heading to $5.4 billion in annual revenue.
Monday, March 2, 2015
Would you swipe left on a healthier you?
2015 health IT innovation holds the promise of turning massive amounts of personal health data into usable information that can keep you healthier -- and it's conveniently accessible on your phone.
It’s always comical to watch movies from the 1980s, not only for the distinct style choices that typified that decade, but to see the type of technology most of us can still recall using. It’s nearly impossible to believe we used to happily lug around three pound mobile phones with antennas and back-up battery packs, but they offered a convenience the likes of which we had never seen before. While heading to the 2015 Mobile World Congress (MWC)
one of the most prominent tradeshows in the tech industry, I couldn’t help but think about the pace of change and get excited about the digital health innovations that will be showcased.
We tend to take for granted the conveniences and time-saving effects such innovation has on our lives. Prior to the pervasiveness of mobile technology, if you were walking down the street and you saw someone collapse, you would need to find the nearest store or phone booth to call for help. In fact, most of us probably knew which corners on our daily commute had pay phones. Now, even if you’ve left your phone in the car (an unthinkable these days) you can comfortably rely on the fact that someone nearby will have theirs in the case of an emergency.
From a healthcare perspective, the interconnectivity of devices is fascinating and holds a lot of potential for engaging patients and improving health outcomes. Innovations such as smart watches, which are being outfitted with fitness trackers and heart rate monitoring sensors, can alert the wearer he has achieved 10,000 steps that day or that a runner has reached her target heart rate
While innovations such as these are always exciting, the bigger picture is about creating a healthier population. According to the World Health Organization, cardiovascular disease is the number one cause of death in the world today. Factors such as poor diet and lack of physical activity are some of the main contributors to the disease— and they are also elements most of us struggle to balance. In other words Lifestyle is the biggest contributor to your health as you can see in this video
Wearable devices designed with intuitive interfaces hold the possibility of helping us maintain that balance, remind us of our inactivity, track our daily caloric intake, remind us of how many hours, minutes, and days it has been since our last cigarette (even Spock spoke out against smoking)
When smart watches and fitness bands are tethered to mobile devices, we can layer on more practical applications for personal health management. What if you were walking down the street and your wearable could sense you were having a minor heart arrhythmia, send a signal to your phone, and have it call for help or advice? Or, perhaps, much like our phones can now alert us to poor traffic for our daily commute, what if your wearable, knowing you are diabetic, could sense low blood sugar, sync this data with your phone and tell you some appropriate restaurants and grocery stores nearby? They will be able to translate personal health data into steps and actions we, as patients, can take to better manage our care and keep ourselves healthier.
We’ve come a long way from the shoe-box sized mobile phones of the ‘80s and it will be interesting to see a glimpse of our future technologies, widgets and devices on display at CES 2015. One thing is certain: whether you’re a physician or a patient, we’re all still consumers and our expectations for efficiency and conveniences on mobile devices will play a large role in the next phase our health evolution. In fact, I imagine the current wearable will be considered clunky and dated in as little as 10 years. We might find our lives equipped with even more svelte tools integrated with all of our healthcare data and real-time advisors, apps or avatars that coach, coerce or cheer us on through daily choices to keep our lives and health on the ideal track.
The original article appeared in WhatsNext
It’s always comical to watch movies from the 1980s, not only for the distinct style choices that typified that decade, but to see the type of technology most of us can still recall using. It’s nearly impossible to believe we used to happily lug around three pound mobile phones with antennas and back-up battery packs, but they offered a convenience the likes of which we had never seen before. While heading to the 2015 Mobile World Congress (MWC)
one of the most prominent tradeshows in the tech industry, I couldn’t help but think about the pace of change and get excited about the digital health innovations that will be showcased.
We tend to take for granted the conveniences and time-saving effects such innovation has on our lives. Prior to the pervasiveness of mobile technology, if you were walking down the street and you saw someone collapse, you would need to find the nearest store or phone booth to call for help. In fact, most of us probably knew which corners on our daily commute had pay phones. Now, even if you’ve left your phone in the car (an unthinkable these days) you can comfortably rely on the fact that someone nearby will have theirs in the case of an emergency.
Is your heart in it?
From a healthcare perspective, the interconnectivity of devices is fascinating and holds a lot of potential for engaging patients and improving health outcomes. Innovations such as smart watches, which are being outfitted with fitness trackers and heart rate monitoring sensors, can alert the wearer he has achieved 10,000 steps that day or that a runner has reached her target heart rate
While innovations such as these are always exciting, the bigger picture is about creating a healthier population. According to the World Health Organization, cardiovascular disease is the number one cause of death in the world today. Factors such as poor diet and lack of physical activity are some of the main contributors to the disease— and they are also elements most of us struggle to balance. In other words Lifestyle is the biggest contributor to your health as you can see in this video
Wearable devices designed with intuitive interfaces hold the possibility of helping us maintain that balance, remind us of our inactivity, track our daily caloric intake, remind us of how many hours, minutes, and days it has been since our last cigarette (even Spock spoke out against smoking)
When smart watches and fitness bands are tethered to mobile devices, we can layer on more practical applications for personal health management. What if you were walking down the street and your wearable could sense you were having a minor heart arrhythmia, send a signal to your phone, and have it call for help or advice? Or, perhaps, much like our phones can now alert us to poor traffic for our daily commute, what if your wearable, knowing you are diabetic, could sense low blood sugar, sync this data with your phone and tell you some appropriate restaurants and grocery stores nearby? They will be able to translate personal health data into steps and actions we, as patients, can take to better manage our care and keep ourselves healthier.
Engagement ROI
The benefits of an engaged patient population are numerous. Not only will people be healthier, but consider the above World Health Organization cardiovascular disease statistics and the associated costs of care, medication, and lost productivity, not to mention the personal impact on each of us. For coronary heart disease alone, the U.S. spends $108.9 billion. If people were more dialed in to their health— tracking, monitoring, and being rewarded by insurance companies for adherence to healthy lifestyle activities— imagine the savings both in lives and dollars. And with the pervasiveness of health IT innovation, we are seeing more consumer-facing health apps, such as Sharecare’s AskMD, becoming standard features on mobile devices. People can now use these apps to walk them through their symptoms, offer guidance on managing chronic conditions, and remind them to check in with their doctors.We’ve come a long way from the shoe-box sized mobile phones of the ‘80s and it will be interesting to see a glimpse of our future technologies, widgets and devices on display at CES 2015. One thing is certain: whether you’re a physician or a patient, we’re all still consumers and our expectations for efficiency and conveniences on mobile devices will play a large role in the next phase our health evolution. In fact, I imagine the current wearable will be considered clunky and dated in as little as 10 years. We might find our lives equipped with even more svelte tools integrated with all of our healthcare data and real-time advisors, apps or avatars that coach, coerce or cheer us on through daily choices to keep our lives and health on the ideal track.
The original article appeared in WhatsNext
Monday, January 26, 2015
Will 2015 be the year your watch teaches you about your health?
There is no known medical condition that enables an individual to predict the future. While such an ability would be extremely useful for myriad reasons, we have, instead, learned to hone and leverage our analytic skills to deduce what might occur, relying on the data we cull and parse to help forecast the future. So, when it comes to predicting the year ahead, we should consider the one we just had.
Regardless of which side of the exam table you sit, we’re all healthcare consumers
Consumer technology is often a good indicator of what type of capabilities and functionalities might be in store for health IT. This past year, we saw major players in the tech space announce their forays into healthcare. While this will not be without its challenges, it does not diminish the underlying fact that there is a need and want for better technology in healthcare— regardless of whether you are a patient looking to effectively manage your weight or a physician struggling to juggle patient care and administrative duties.
In the last year, we saw a wave of next-generation wearable devices flood the market, and as a result, we, as patient consumers, now have streamlined access to information such as our daily step count and average heart-rate on our watches. We know that ease-of-use, understandability, and some level of gameification:
“Congratulations! You’ve reached your target heart rate today!”
are vital to maintaining engagement.
I believe this is the beginning of something much larger, a groundswell movement that will result in patients wanting more information about their health data, and, more importantly, craving a better understanding of what all these numbers actually mean and how to positively impact them. Achieving this level of engagement demands a simpler intelligent interface that doesn’t require a learning curve, but is one that consumers can just use. Clever user interface designs can only go so far, particularly given the small visual real estate available on wearable devices, and the addition of capabilities such as intelligent voice assistants will be an integral part of this explosion of personal health management.
Having a heart-to-heart about your heart
Technology holds the potential to create clinical synergy, bringing patient consumers (who have become professional health IT consumers, or health prosumers) better intelligence about their personal health data and outlining the proactive measures they can take to become better partners in their own health. The average patient consumer may not have a reaction to the phrase“Your Protime this week is 3.3,” but for someone with a heart condition, this number is very important and indicates how fast her blood is clotting. The data, while extremely useful to a clinician, is only helpful to the patient if she understands what it means and how she can take the right actions as a result.
The future is about patients managing their own care and working alongside clinicians to drive better outcomes. To the woman who has a Protime of 3.3, access to these results supplemented with clinical guidelines would mean that she wouldn’t need to wait for her physician to call with diet recommendations, she would know her blood is clotting too slowly and that she might have an inadequate protein consumption or might need to increase her vitamin K intake. If the number required that her Coumadin dosage be adjusted, this would be the point where her physician would reach out to her to discuss.
Although a basic example, it is one that has endless permutations when it comes to building a more engaged patient population. There is no one more invested in your health than you, and the person who cares the next most about keeping you well, is your physician. I believe that clinical synergy will be driven by both patients, who want to actively manage their chronic conditions and take meaningful preventative care measures, and physicians who want to empower their patients to better understand how the choices they make have significant health implications. Technology is the connective fiber that can enable the transmission of this important data, and help translate it into wisdom. And that truly is the crux—the data flowing between patient and physician must be relevant and meaningful. That ability for technology to determine the relevancy of health data information is just around the corner and soon our wearables will be able to notify our health information data that deviates from our personal “normal” results.
Approximately 75 percent of U.S. healthcare expenditure is related to chronic care management, imagine the impact this level of clinical synergy will have on driving a healthier population while reducing cost. I’m ready, are you?
This post originally appeared on WhatsNext
Tuesday, November 11, 2014
Bridging the Digital DIvide
This week I will be at the Medicine 2.0 Conference on a panel Bridging the Patient Digital Divide moderated by
Melody Smith Jones
and includes
Lauren Still
and
Nick Genes
The session was put together by Melody to take on the oft talked about but perhaps poorly understood “Digital Divide”. Patients spend less than 1% of their time with doctors - the balance of our time represents (lost) opportunity to interact with people helping them live fulfilling healthy lives and making the best possible choices.
But there is variability with access in the community to information technology preventing access and knowledge and skills necessary to derive the value from these tools. Melody has addressed this divide specifically focusing on apps doe Low-Income Mothers in her recent post: 3 High Health Apps for Low-Income Moms. Check out Melody’s top 3 picks for low income mothers - some great apps focusing on the Food stamps including clever use of Bar code scanning technology to check eligibility of food and the nutritional value and a novel use of simple text messaging to improve maternal and newborn health <----- approach="" font="" love="" of="" simplicity="" the="" this="">
As she points out many of us make assumptions about accessibility to technology in lower social economic groups- as she puts it
Out of the world’s estimated 7 billion people, 6 billion have access to mobile phones. Only 4.5 billion have access to working toilets.
In one of my personal areas of passion - Africa that is replete with examples of successful use of technology to impact the health of the population at levels that we can only dream of here in “the West". Here in this study: Text message reminders improve healthcare practice in rural Africa
and this piece in the Atlantic: Medicine by Text Message: Learning From the Developing World
It might seem counter intuitive to spend money on what some might consider a luxury or discretionary spend - but for some this is the only means of communication replacing the plain old telephone line (POTS) and these devices come with capabilities and a reach that was pervasively unavailable to many in our society. The statics suggest as many as 80% of low income consumers own a mobile device.
But despite this opportunity the technology and apps are often times targeted at the higher income who already have fitter healthier lifestyles. Some of this is because of the existing developer community (higher social economic group) who develop for the problems they perceive and the harsh economics - this is where the money is (or at least we think it is). Despite Malaria being such a big killer there is limited investment in prevention and treatment of the disease as it affects the poor nations with limited capacity to buy any solutions that are developed despite significant progress and the impact of World Malaria Day
This was covered eloquently by J.C. Herz at wired in this piece: Wearables Are Totally Failing the People Who Need Them Most. We are awash with wearables, new devices and new apps and buckling under a Tsunami of data but:
I’m with Kabir Kasagood, director of business development for Qualcomm Life who said
Melody Smith Jones
and includes
Lauren Still
and
Nick Genes
The session was put together by Melody to take on the oft talked about but perhaps poorly understood “Digital Divide”. Patients spend less than 1% of their time with doctors - the balance of our time represents (lost) opportunity to interact with people helping them live fulfilling healthy lives and making the best possible choices.
On average, patients only spend 1% of their time in the clinical care setting. Traditional medicine has focused upon patient engagement during that eight minute doctor visit. Yet, it is the other 99% of the time, when patients are at home, at work, at school, and in their communities that matters most. It is outreach to patients while they are living, working, and playing that determines how their overall wellness is managed.We have seen a plethora of technologies that attempt to address this area with everything from diet and fitness apps to specific applications designed to address long term health issues.
But there is variability with access in the community to information technology preventing access and knowledge and skills necessary to derive the value from these tools. Melody has addressed this divide specifically focusing on apps doe Low-Income Mothers in her recent post: 3 High Health Apps for Low-Income Moms. Check out Melody’s top 3 picks for low income mothers - some great apps focusing on the Food stamps including clever use of Bar code scanning technology to check eligibility of food and the nutritional value and a novel use of simple text messaging to improve maternal and newborn health <----- approach="" font="" love="" of="" simplicity="" the="" this="">
As she points out many of us make assumptions about accessibility to technology in lower social economic groups- as she puts it
Many make an assumption that those with low income or low education levels would not have mobile technology to use in the first placeBut despite the budgetary restrictions we see a very high level of adoption of mobile technology - this is true worldwide as demonstrated by the statistics of mobile phone in the world: More People Have Cell Phones Than Toilets, U.N. Study Shows.
Out of the world’s estimated 7 billion people, 6 billion have access to mobile phones. Only 4.5 billion have access to working toilets.
In one of my personal areas of passion - Africa that is replete with examples of successful use of technology to impact the health of the population at levels that we can only dream of here in “the West". Here in this study: Text message reminders improve healthcare practice in rural Africa
and this piece in the Atlantic: Medicine by Text Message: Learning From the Developing World
It might seem counter intuitive to spend money on what some might consider a luxury or discretionary spend - but for some this is the only means of communication replacing the plain old telephone line (POTS) and these devices come with capabilities and a reach that was pervasively unavailable to many in our society. The statics suggest as many as 80% of low income consumers own a mobile device.
But despite this opportunity the technology and apps are often times targeted at the higher income who already have fitter healthier lifestyles. Some of this is because of the existing developer community (higher social economic group) who develop for the problems they perceive and the harsh economics - this is where the money is (or at least we think it is). Despite Malaria being such a big killer there is limited investment in prevention and treatment of the disease as it affects the poor nations with limited capacity to buy any solutions that are developed despite significant progress and the impact of World Malaria Day
This was covered eloquently by J.C. Herz at wired in this piece: Wearables Are Totally Failing the People Who Need Them Most. We are awash with wearables, new devices and new apps and buckling under a Tsunami of data but:
...developers continue flocking to a saturated market filled with hipster pet rocks, devices that gather reams of largely superficial information for young people whose health isn’t in question, or at risk. It’s a shame because the people who could most benefit from this technology—the old, the chronically ill, the poor—are being ignored. Indeed, companies seem more interested in helping the affluent and tech-savvy sculpt their abs and run 5Ks than navigating the labyrinthine world of the FDA, HIPAA, and the other alphabet soup bureaucracies.There are some economic reasons for these current trends, some social aspects of the development community but these may be based on false belief of the economics when you consider the opportunity exists to shake up the $2 trillion annual cost of chronic disease….!
I’m with Kabir Kasagood, director of business development for Qualcomm Life who said
Go from the children’s table to the grown-up table...If you’re serious about this, embrace the FDA. Learn how HIPAA works... move away from fitness and go hardcore into health. That’s where the money isAround 45% of US adults are dealing with at least on chronic condition and picking on one Diabetes and look at the market opportunity of $6.3 Billion spent on blood glucose strips gives you a sense of the economics of this market. These are motivated people for whom the quantified self can mean the difference between an (expensive) admission to hospital or managing and improving at home.
At some point, you’ve got to ask yourself whether it’s just the friction created by health-industry regulation—the HIPAA security rules and FDA approval (or waiver) process and the hassle of integration with legacy systems. Or is it too daunting for a twenty-something engineer to develop technology for people who aren’t like them at all? An obese diabetic on a motorized scooter? Or a frail old lady with memory loss? Or her caregiver? Someone who’s three bus transfers away from a doctor’s office?We plan to address these issues in our panel - if you can’t join us maybe you can join the conversation using the hash tag from the conference #Med2 here at Symplur
Monday, October 27, 2014
The #EMR, #Ebola and #Bigdata - what Can We Learn
After all the hype and knee jerk politics and media I was delighted to read this piece Ebola US Patient Zero: lessons on misdiagnosis and effective use of electronic health records by Upadhyay, Sittig and Singh (PDF file here)
A thoughtful piece that drilled in to the detail of events surrounding the arrival and subsequent consultations, admission and treatment of Thomas Eric Duncan
who sadly died on October 8 succumbing to the ravages of the Ebola virus
As the authors state
The authors used the publicly available documents and testimony in their quest and it is important to note that they did not have access to the full record, the EMR used or indeed all the pieces of the puzzle and made up for this in some areas with educated guesses.
It is interesting to note that in the first visit to the ED the patient's temperature spiked to 103 degrees accompanied by pain described by the patient as 8/10 in severity.
He was diagnosed on initial discharge included sinusitis but "but that CT scans of “head and abdomen” ordered during the ED visit showed no evidence of sinusitis" and perhaps with more attention and importantly time made available to the clinical staff would offer them the opportunity to focus on the history and examination and less on high tech investigation. In many cases clinicians are forced into their use not by clinical practice but rather to meet the production pressures - as the authors put it
As for the process of information capture - we have lost site of the information that is relevant in the fog of billing and regulatory driven template driven charting.
not "EHRs can lead to less verbal exchange" - EHRs do lead to less verbal exchanges
The data entry requirements place an enormous burden on our clinical professionals
who are tasked and measured not on clinical practice and the delivery of great care but on specific content of documentation that is mandated to capture clinical information in specific ways determined by the reimbursement, coding and regulatory system.
Technology can help but there are some fundamental flaws in the design and management of healthcare that are fed by the current incentives. Many initiatives attempting to improve patient safety and value-based purchasing but don't focus on accuracy and timeliness of diagnosis and in particular Outpatient reimbursement policies do not reward diagnostic decision-making, teamwork, or quality time spent with the patient in making a diagnosis.
What you incent is what you get and this needs to be changed as well.
A thoughtful piece that drilled in to the detail of events surrounding the arrival and subsequent consultations, admission and treatment of Thomas Eric Duncan
who sadly died on October 8 succumbing to the ravages of the Ebola virus
As the authors state
The mishandling of US Patient Zero is receiving widespread media attention highlighting failures in disaster management, infectious disease control, national security, and emergency department (ED) care.....also brought decision-making vulnerabilities in the era of the Electronic Health Record (EHR) into the public eyeMuch of the commentary generated "fear, uncertainty, and doubt about the competence of our health care delivery system" and while there were problems I agree with the authors that this is a “teachable moment” and a chance to identify the missed opportunities and key issues that we can learn from
The authors used the publicly available documents and testimony in their quest and it is important to note that they did not have access to the full record, the EMR used or indeed all the pieces of the puzzle and made up for this in some areas with educated guesses.
It is interesting to note that in the first visit to the ED the patient's temperature spiked to 103 degrees accompanied by pain described by the patient as 8/10 in severity.
| This from a Malaria Study but typical of the Spike in Temperature found with this disease |
He was diagnosed on initial discharge included sinusitis but "but that CT scans of “head and abdomen” ordered during the ED visit showed no evidence of sinusitis" and perhaps with more attention and importantly time made available to the clinical staff would offer them the opportunity to focus on the history and examination and less on high tech investigation. In many cases clinicians are forced into their use not by clinical practice but rather to meet the production pressures - as the authors put it
A host of system-related factors detract from optimal conditions for critical thinking in the ED, leading clinicians to lose situational awareness. These include production pressures, distractions, and inefficient processesThe upshot was a discharge and subsequent return days later at and even then:
even after the second ED visit which led to hospitalization, strict Ebola isolation precautions were not followed for 2 days, until the diagnosis was confirmed by the CDCOffering a window into the events that is made so much easier with the benefit of 20/20 hindsight
The authors offer some learning opportunities that are worth highlighting
Top of the list in would be working with software developers to improve EHR usabilityAs this case illustrates, EHR-based clinical workflows often fail to optimize information sharing amongst various team members, leading to lapses in recognizing specific clinical findings that could aid in rapid and accurate diagnosisAs an interesting addition none of the systems (or incentives) have any form of feedback loop built in to allow clinicians to learn from their actions.
As for the process of information capture - we have lost site of the information that is relevant in the fog of billing and regulatory driven template driven charting.
Condition-specific charting templates, drop-down selection lists, and checkboxes developed in response to billing or quality reporting requirements potentially distort history-taking, examination, and their accurate and comprehensive recording.. Clinicians also tend to ignore template-generated notes in their review process; often the signal-to-noise ratio in these notes is low. EHRs can lead to less verbal exchange, which is all the more needed and more effective when dealing with complex tasks and communicating critical informationRight on except to say this does not "potentially distort history-taking" - it does distort history-taking and
not "EHRs can lead to less verbal exchange" - EHRs do lead to less verbal exchanges
The data entry requirements place an enormous burden on our clinical professionals
who are tasked and measured not on clinical practice and the delivery of great care but on specific content of documentation that is mandated to capture clinical information in specific ways determined by the reimbursement, coding and regulatory system.
Other factors, such as heavy data entry requirements and frequent copy-and-paste from previous notes, detract from critical thinking during the diagnostic decision-making process... For EHRs to be most effective, they need to be able to automatically sort through patient data, identify the pertinent findings, and present them in an easy to understand manner. Computer algorithms could combine patient-specific information with the latest evidence-based clinical knowledge to help clinicians reach the correct diagnosisThis is the next frontier of Healthcare technology and in particular clinical documentation - we know we can sort through patient data, identify the pertinent findings - focused in these examples on quality of care and evidence based guidelines and we know computer algorithms can use patient specific information combined with evidence based knowledge to help
Technology can help but there are some fundamental flaws in the design and management of healthcare that are fed by the current incentives. Many initiatives attempting to improve patient safety and value-based purchasing but don't focus on accuracy and timeliness of diagnosis and in particular Outpatient reimbursement policies do not reward diagnostic decision-making, teamwork, or quality time spent with the patient in making a diagnosis.
What you incent is what you get and this needs to be changed as well.
Thursday, August 14, 2014
Speech and the Digital healthcare Revolution at #SpeechTek
Come join me in the conversation with my colleagues at the SpeechTek 2014 conference in Marriott Hotel in Time Square, Manhattan New York.
The Panel: C103 – PANEL: The Digital Healthcare Revolution at 1:15 p.m - 2:00 p.m. The panel moderator Bruce Pollock, Vice-President, Strategic Growth and Planning at West Interactive and on Social Media @brucepollock
I will be joined by Daniel Padgett, Director, Voice User Experience at Walgreens and on Social Media at @d_padgett and David Claiborn, Director of Service Experience Innovation at United Health Group.
We will be discussing the opportunities and challenges associated with the current digital healthcare revolution and of course how speech plays an essential role in integrating this technology while maintaining the human component of medicine that we all want. Rather than Neglecting the patient in the era of health IT and EMR
We have progressed from the world of Sir Lancelot Spratt
And the Doctor need to look at the patient not the technology perhaps in a cooperative Digital Health world like this
Is this future of Virtual Assistant Interaction good, desirable
Demo Video 140422 from Geppetto Avatars on Vimeo.
We will be discussing
Perhaps the emerging Glass concepts improve this interaction as they are exploring in Seattle
Join us for analysis of the state of digital healthcare today and predictions for its future.
In the end
Come join the discussion as we explore the digital technology and how it should be used in healthcare and how speech can help
The Panel: C103 – PANEL: The Digital Healthcare Revolution at 1:15 p.m - 2:00 p.m. The panel moderator Bruce Pollock, Vice-President, Strategic Growth and Planning at West Interactive and on Social Media @brucepollock
I will be joined by Daniel Padgett, Director, Voice User Experience at Walgreens and on Social Media at @d_padgett and David Claiborn, Director of Service Experience Innovation at United Health Group.
We will be discussing the opportunities and challenges associated with the current digital healthcare revolution and of course how speech plays an essential role in integrating this technology while maintaining the human component of medicine that we all want. Rather than Neglecting the patient in the era of health IT and EMR
We have progressed from the world of Sir Lancelot Spratt
And the Doctor need to look at the patient not the technology perhaps in a cooperative Digital Health world like this
Is this future of Virtual Assistant Interaction good, desirable
Demo Video 140422 from Geppetto Avatars on Vimeo.
We will be discussing
- What are the biggest obstacles to digital healthcare becoming a reality?
- Where do speech technologies bring the most value to healthcare?
- How will health providers, insurers, and payers provide patient support in the world of digital healthcare?
Perhaps the emerging Glass concepts improve this interaction as they are exploring in Seattle
Join us for analysis of the state of digital healthcare today and predictions for its future.
In the end
People forget what you said and what you did but they remember how you made them feel
Come join the discussion as we explore the digital technology and how it should be used in healthcare and how speech can help
Friday, July 18, 2014
Wearable Technology - An Exploding Segment
I attended a Wearble Technology conference today in Pasadena California: Wearable Tech LA
There was a wide range of technologies and innovations - everything from the mind monitoring by IntraXon’sMuse headband. Here’s their online demo video
One of the more interesting concepts takes the challenge we have all faced mastering the mechanics of walking, exercise, running and in some cases rehabilitation by placing sensors in the sole of shoes - Plantiga who have taken force analysis for our feet to a whole new level
The technology takes the static Force Plate sensor and turns into a continuous assessment 3-D tool offering an opportunity to apply this in specific sports and to help rehabilitate people who have been injured or have mechanical challenges (the side effect of capturing all this data is actually creating more comfortable shoes as they now have built in suspension and springs).
It might take a while to arrive in healthcare but in the meantime may well show up as another input device for the X-box or PS3 for a more realistic interface.
There was sensors to be placed all over the body for respiration, heart rate, muscle movement, acceleration/deceleration and even some to be ingested
A major challenge highlighted by several speakers facing all of the wearables genre was the issue of battery life
(and ironically it was the same problem I faced as I tried to capture and post social media)
The opening keynote was from Nadeem Kassam - CEO of BioBeats (Founder of Basis which is now an Intel company). His journey was one of classic rise from poor neighborhood in South Africa where he started his entrepreneur sporty selling oranges
He focused on three lessons - the first an essential learning point for everyone especially those facing healthcare challenges
He also suggested that those looking to succeed with innovation should:
His story behind this was a classic one of engineers told to build a product who came back with his wearable watch that was a huge device that weighed down his arm and had a velcro battery pack under the arm!
He ended up finding his greatest engineers on Craigslist who’s references and Resume was a cardboard box full of devices that he had built.
The new concept of “Adaptive Media” which is bridging the divide between human emotion, data and the media we consume and should adapt to our mood based on our emotion. His new company has done some interesting research programs including an experiment with machines designed to allow people to hear their own heartbeat and have it set to music in Australia. When people heard their heartbeat for the first time it created a deeply emotional experience and many were moved to share very personal life stories.
They took this a step further and worked to gather heartbeats worldwide - a clever BIGData gathering exercise that amassed large quantities of rate, rhythm and details of millions of people around the world.
His overriding point was
There was a fascinating blend of the Entertainment industry and Hollywood and a slew of companies taking different approaches to these devices:
Epihany Eyewear tries to make wearables fashionable as well as functional (I’d say it not so much as fashion but blending into society)
Optivent with powerful wearable glass - but no mention of the interface
They probably had the most fun concept video
Les lunettes d’Optinvent voient plus grand que les Google glass from Rennes, Ville et Métropole on Vimeo.
Enlightened design had the most impressive on stage display with a jacket that had lapels that constantly changing color
Sporting her jacket with lapels that constantly changed color
Given the excitement over the last month wight he World Cup it was fascinating to hear from Stacey Burr from Adidas who revealed that most if not all the teams were using technology to help them train and track in extensive detail - she suggested that there is not a single team or sport that is not using wearable technology in some form or another.
You can see some of the gear below
These are the professional versions used by major teams but Adidas is releasing commercial versions that will be available to the general public but lack the GPS capability and the analysis tools they offer
Surprisingly the leaders from a sports and country standpoint are Rugby and Australia and New Zealand who are "light years ahead" of wearable tech in sports
Sensoria demonstrated an exciting interactive future for sports and wearables where we challenge ourselves, other people and are coached by virtual assistants
Sensoria Fitness Shirt with Heart Rate Sensors from Heapsylon on Vimeo.
One of the highlights:Seeing Dick Fosbury of the "Fosbury Flop” Olympic Gold Medal Winner from Mexico 1968 and it turns out he is a Cancer Survivor, has an aneurysm and fully engaged in the intersection between healthcare and wearable technology
Neil Harbisson - Co-Founder, Cyborg Foundation
who was born totally color blind was definitely at the edge of wearable technology. He has an implanted device that turns color into sound and this is directly fed into his brain. He described that it took 5 weeks for the headaches to stop with this sudden input of data and then 5 months before it just became part of him and he now sees in color.
Here's his TED Talk: I listen in Color
He also has a permanent internet connection in his brain so people cane send him colors and images directly (he joked the address is private - but I did wonder given the ease with which spammers seem to find new addresses how he protects this destination from spam!)
OMSignal (Jesse Slade Shantz - Chief Medical Officer) was the most interesting as they are trying to change the monitoring from attached sensors to using fabric that can be loose fitting but can capture physiological information.
Breathometer (Charles Michael Yim - CEO) focus on analyzing your breath and have a range of products directed at health (over and above their simplistic alcohol breathalyzer available today) that assessed fat burning (using acetone) and asthma
NeuroSky (Stanley Yang - CEO) offer a system that other manufacturers can integrate into their wearables. Typically found in mobile phones or headsets
LUMO (Monisha Perkash - CEO & Co-founder) offering a discreet sensor that is designed to help improve your body posture and works as a tracker.
It's an exciting future with some fascinating technology to come - one thing for sure - with ubiquitous technology comes ubiquitous complexity and your voice will become an essential tool for successfully managing and navigating. Dragon Assisatnt is one of several tools built to assist in using and navigating technology that is reinventing the relationship between people and technology
There was a wide range of technologies and innovations - everything from the mind monitoring by IntraXon’sMuse headband. Here’s their online demo video
One of the more interesting concepts takes the challenge we have all faced mastering the mechanics of walking, exercise, running and in some cases rehabilitation by placing sensors in the sole of shoes - Plantiga who have taken force analysis for our feet to a whole new level
The technology takes the static Force Plate sensor and turns into a continuous assessment 3-D tool offering an opportunity to apply this in specific sports and to help rehabilitate people who have been injured or have mechanical challenges (the side effect of capturing all this data is actually creating more comfortable shoes as they now have built in suspension and springs).
Better than this concept!
It might take a while to arrive in healthcare but in the meantime may well show up as another input device for the X-box or PS3 for a more realistic interface.
There was sensors to be placed all over the body for respiration, heart rate, muscle movement, acceleration/deceleration and even some to be ingested
A major challenge highlighted by several speakers facing all of the wearables genre was the issue of battery life
(and ironically it was the same problem I faced as I tried to capture and post social media)
The opening keynote was from Nadeem Kassam - CEO of BioBeats (Founder of Basis which is now an Intel company). His journey was one of classic rise from poor neighborhood in South Africa where he started his entrepreneur sporty selling oranges
He focused on three lessons - the first an essential learning point for everyone especially those facing healthcare challenges
Nothing is stronger than habit
He also suggested that those looking to succeed with innovation should:
- Look for innovation outside of your industry, and
- Don’t throw a big team or money at innovation
His story behind this was a classic one of engineers told to build a product who came back with his wearable watch that was a huge device that weighed down his arm and had a velcro battery pack under the arm!
He ended up finding his greatest engineers on Craigslist who’s references and Resume was a cardboard box full of devices that he had built.
The new concept of “Adaptive Media” which is bridging the divide between human emotion, data and the media we consume and should adapt to our mood based on our emotion. His new company has done some interesting research programs including an experiment with machines designed to allow people to hear their own heartbeat and have it set to music in Australia. When people heard their heartbeat for the first time it created a deeply emotional experience and many were moved to share very personal life stories.
They took this a step further and worked to gather heartbeats worldwide - a clever BIGData gathering exercise that amassed large quantities of rate, rhythm and details of millions of people around the world.
His overriding point was
We have to make health fun and engaging - merging it with entertainment to help people achieve what we all want - long tail of healthy life
Epihany Eyewear tries to make wearables fashionable as well as functional (I’d say it not so much as fashion but blending into society)
Optivent with powerful wearable glass - but no mention of the interface
They probably had the most fun concept video
Les lunettes d’Optinvent voient plus grand que les Google glass from Rennes, Ville et Métropole on Vimeo.
Enlightened design had the most impressive on stage display with a jacket that had lapels that constantly changing color
 |
| Janet Hansen - Founder & Chief Fashion Engineer, Enlightened Designs |
Sports and Wearable
Given the excitement over the last month wight he World Cup it was fascinating to hear from Stacey Burr from Adidas who revealed that most if not all the teams were using technology to help them train and track in extensive detail - she suggested that there is not a single team or sport that is not using wearable technology in some form or another.
You can see some of the gear below
 |
| GPS enabled ECG/EKG monitoring Units plug into the back around the neck area |
 |
| Paired with watches to offer players feedback |
 |
| Digital insides of a ball used to sense how well it is struck |
These are the professional versions used by major teams but Adidas is releasing commercial versions that will be available to the general public but lack the GPS capability and the analysis tools they offer
Surprisingly the leaders from a sports and country standpoint are Rugby and Australia and New Zealand who are "light years ahead" of wearable tech in sports
| They are ahead in Psyching out their opponents too! |
Sensoria demonstrated an exciting interactive future for sports and wearables where we challenge ourselves, other people and are coached by virtual assistants
Sensoria Fitness Shirt with Heart Rate Sensors from Heapsylon on Vimeo.
One of the highlights:Seeing Dick Fosbury of the "Fosbury Flop” Olympic Gold Medal Winner from Mexico 1968 and it turns out he is a Cancer Survivor, has an aneurysm and fully engaged in the intersection between healthcare and wearable technology
Neil Harbisson - Co-Founder, Cyborg Foundation
who was born totally color blind was definitely at the edge of wearable technology. He has an implanted device that turns color into sound and this is directly fed into his brain. He described that it took 5 weeks for the headaches to stop with this sudden input of data and then 5 months before it just became part of him and he now sees in color.
Here's his TED Talk: I listen in Color
He also has a permanent internet connection in his brain so people cane send him colors and images directly (he joked the address is private - but I did wonder given the ease with which spammers seem to find new addresses how he protects this destination from spam!)
I don't wear technology I am technology, I can't tell the difference between the software & my brain
The healthcare focused panel: Emerging Wearable 2.0 Health Platforms:
The furthest along and well know was probably Misfit wearables (Sonny Vu, CEO) who try and make sensors “disappear” but still simple sensorsOMSignal (Jesse Slade Shantz - Chief Medical Officer) was the most interesting as they are trying to change the monitoring from attached sensors to using fabric that can be loose fitting but can capture physiological information.
Breathometer (Charles Michael Yim - CEO) focus on analyzing your breath and have a range of products directed at health (over and above their simplistic alcohol breathalyzer available today) that assessed fat burning (using acetone) and asthma
NeuroSky (Stanley Yang - CEO) offer a system that other manufacturers can integrate into their wearables. Typically found in mobile phones or headsets
LUMO (Monisha Perkash - CEO & Co-founder) offering a discreet sensor that is designed to help improve your body posture and works as a tracker.
It's an exciting future with some fascinating technology to come - one thing for sure - with ubiquitous technology comes ubiquitous complexity and your voice will become an essential tool for successfully managing and navigating. Dragon Assisatnt is one of several tools built to assist in using and navigating technology that is reinventing the relationship between people and technology
Tuesday, May 27, 2014
Getting Value from the EHR - Yes it is Possible
I have the privilege of spending a lot of time on the road interacting with clinicians around the country (and world). I hear with too much frequency many doctors complaining about the Electronic Medical Record and how it fails to help them and in many cases makes their work harder. Some of this is a hangover from the past and the inadequate technology and in some cases hardware at the time
In fact I’ve told this story a number of times that I can date to around 1995/6 and in this piece: Clinical documentation in the EHR
This article on Government HealthIT Are electronic health records already too cluttered? highlights a rising problem and one I hear about frequently. This is not just a healthcare problem and it is the focus of the work by Edward Tufte an American statistician and professor emeritus of political science, statistics, and computer science at Yale University who is well known for his books on information design which are bets acquired by attending one of his frequent courses on data visualization
Here is a recent overview of visualization on the iPhone
He has a section on healthcare but many of his principles apply
For Brian Jacobs the problem was even more acute working in a Pediatric ICU:
So they instituted a policy of One Note per day
Actually its
So in addressing the issue clutter they also addressed usability and design turning the note into a living breathing document that is updated and maintained by the team that now takes care of patients
But he addressed some other important issues - especially when it comes to quality of care and the quality of the medical note
Copy Forward is subject to some warranted scrutiny from a billing and audit standpoint. Much of the repetitive and “clutter” in the note comes form the copying forward of past information. But:
Add to that an updated and well maintained Problem List and integration with the billing system to allow doctors to select their code for the work carried out that day and they moved to a valuable addition to the healthcare team in delivering quality healthcare with their EHR
In fact I’ve told this story a number of times that I can date to around 1995/6 and in this piece: Clinical documentation in the EHR
Many years ago, an excited friend who worked for one of the electronic health record (EHR) vendors at that time — it was really more of a billing and patient tracking and management system than an EHR — was desperate to show me some of their latest applications. In particular, a new module they had developed to capture clinical data.There is still some of that going on and not enough focus on the User Interface design and turning the technology into a barrier - this is the focus of the Art of Medicine campaign we launched some weeks ago
My friend pulled out his laptop, fired up the application, selected a patient and proceeded to enter blood pressure (BP). Some 20-plus clicks later, he had entered a BP of 120/80. While he was excited, I was dumbfounded. When it comes to patient care, doctors didn’t have time for 20 clicks to record BP years ago and they definitely don’t have that luxury in today’s demanding medical environment.
This article on Government HealthIT Are electronic health records already too cluttered? highlights a rising problem and one I hear about frequently. This is not just a healthcare problem and it is the focus of the work by Edward Tufte an American statistician and professor emeritus of political science, statistics, and computer science at Yale University who is well known for his books on information design which are bets acquired by attending one of his frequent courses on data visualization
Here is a recent overview of visualization on the iPhone
He has a section on healthcare but many of his principles apply
For Brian Jacobs the problem was even more acute working in a Pediatric ICU:
The ICU is a very toxic and tech-laden environment….because of that, it offers the opportunity to make a lot of mistakesAs he points out much of the cutter derives form the multiple notes entered into the EHR every day. "It’s not uncommon in teaching hospitals to have six to seven notes per day on one patient, by the time the attending physician, residents, consultants, other doctors and fellows check on the patient."
So they instituted a policy of One Note per day
Actually its
It’s actually one note per team per patient per day; one giant multi-contributor note. They still may be all writing their components, but it’s one noteWith a template to hold the content generated each morning by the resident and then everyone contributing to that one note, adding and amending as necessary
So in addressing the issue clutter they also addressed usability and design turning the note into a living breathing document that is updated and maintained by the team that now takes care of patients
But he addressed some other important issues - especially when it comes to quality of care and the quality of the medical note
Copy Forward is subject to some warranted scrutiny from a billing and audit standpoint. Much of the repetitive and “clutter” in the note comes form the copying forward of past information. But:
These notes should never be the sameAnd as part of that message they moved to an "End-of-day note” that was a fresh summary of the patient.
Add to that an updated and well maintained Problem List and integration with the billing system to allow doctors to select their code for the work carried out that day and they moved to a valuable addition to the healthcare team in delivering quality healthcare with their EHR
EHRs are: more complete, legible, accessible and can be auto-populated and searched. They can provide diagnosis codes and they’re good for billing. On the other hand, they can sometimes lack quality information and are by far, too cluttered.I said this back in 2003 (yikes!) - The Future of Technology is already here - Who’s on Board the train and who’s left at the station. I still believe it and understand that the technology does need to get better and be more integrated into the existing workflow
The next generation of health care technology is here, with visionaries and futurists pushing the envelope to enhance, create and generate the newest cutting edge in health care delivery. Advances in technology, like advances in medicine, are a shared entity that enhances life expectancy and the quality of life.
Wednesday, May 7, 2014
Patients Prefer Electronic Documentation
Software Advice recently published this survey: Do Patients Really Care if You Use Your EHR in the Exam Room? It was very revealing! It turns out contrary to the perception that the intrusion of EMR’s in the office patients prefer electronic documentation to alternatives
What was more surprising was the push back by patients on having scribes
But worst of all - recording devices
There was a big preference to Electronic documentation at the point of care
They asked about reasons for dissatisfaction
Its not the technology that causes the dissatisfaction but in order of importance (for patients)
And coming in with a sliver of dissatisfaction at 5% “Doctor using a Computer in the exam room"
Most Patients Don’t Mind Electronic Note-Taking During ExamsIn each case, more than 80 percent of respondents indicated they would not be bothered. On a sliding scale, patients indicated the least concern for doctors using tablets during the exam.
What was more surprising was the push back by patients on having scribes
But worst of all - recording devices
Ultimately, over one-third of patients said they’d be bothered by doctors using tape recorders to assist in charting medical notes. Specifically, patients at the furthest end of the spectrum—those who chose “would bother me a lot”—were more prevalent when it came to tape recordings than with any other method of charting during an exam.
There was a big preference to Electronic documentation at the point of care
They asked about reasons for dissatisfaction
Its not the technology that causes the dissatisfaction but in order of importance (for patients)
- long wait times at the doctor’s office,
- unfriendly staff
- short duration of visits with the doctor
- Trouble Scheduling Appointment
And coming in with a sliver of dissatisfaction at 5% “Doctor using a Computer in the exam room"
Friday, March 28, 2014
Getting Doctors Back to the Patient - Part 1
The Panel "The Art of Medicine" Panel (part of the Art of Medicine campaign) took place yesterday from 9 - 11am at the Boston's W Hotel, 100 Stuart St, Boston, MA
Our panelists from Left to Right
- John D. Halamka, MD, MS, CIO of Beth Israel Deaconess Medical Center (and Life as healthcare CIO blog and @jhalamka)
- Keith Dreyer, DO, PhD, FACR, Vice Chairman of Department of Radiology, Massachusetts General Hospital
- Adam Landman, MD, MS, MIS, MHS, CMIO, Health Information and Integration at Brigham and Women's Hospital (@landmaad)
- Steven J. Stack, MD, past chair of the American Medical Association (AMA); served on multiple federal advisory groups for ONC on HIT, practicing emergency physician
And it was very well attended:
Today, physicians are struggling to serve their patients’ needs in a healthcare system that seems to work against them at every turn. While technology has the potential to vastly improve healthcare overall, issues remain when it comes to usability, data-entry and complementing patient care vs. competing with it.
In part 1 I have attempted to capture the underlying sentiments and thoughts form our panelists together with some thoughts on potential ways to help resolve these areas and problems.
The panel opened with the original Art of Medicine video:
The session was divided into several separate discussions - the first of which the Issues of today:
There has been an increasing burden placed on physicians to document more and more detail but no additional time to do this and in fact probably less and they struggle with the increasing information over load and the challenge of processing - As John Halamka put it:
"We're already overwhelmed with data, what we need is knowledge & wisdom" @jhalamka@NuanceHealth#artofmedicine
— Stephanie Rufo (@StephRufo27) March 27, 2014
"We need wisdom and today's #EHR make that hard to get from patient info to give me what I need now"
"3 petabytes of patient data...overwhelmed with data, we just need information, knowledge"
This is combined with the increasing regulations which the panel viewed as directly linked to the increasing need for HealthIT tools to help deal with these regulations. As Adam Landmaan put it the design of the EHR’s is based on the design focus and in the current fee for service health system is designed largely support the physicians to capture and document optimize for bill not for patient care
But I thought Keith Dreyer captured the sentiment well when he described technology as decreasing our ability to communicate
“I couldn't imagine dictating into a microphone in talking with my family "
And we are seeing declining capture off the patient’s story in the EHR
Some snapshots of ideas thoughts from our panelists included:
- IT tools driving “note bloat” of information that is non-specific to the patient
- Physicians need timely “wisdom” to positively effect patient care at the time of encounter
- “Big bang” of government funding for EHR adoption has generated massive amounts of information that is, at present, unmanageable
- At stage now of EHRs where they are “one size fits all,” so not customized to specific specialty/setting needs
- Need to identify the smallest number of moving parts (IT tools) to facilitate patient care
- Need for monolithic (“one size fits all”) IT solutions is driven by babel of nomenclature
- Quality measures show that there is a problem, but not the causality
There was much more discussions and thoughts on solutions but one of the concepts that stood out for me was this one from Adam Landmaan straight out of the Television Reality show - copying the Shark Tank concept
That will be an interesting panel and team event and look forward to hearing the results
We need to return to the Art of Medicine and as one panelist put it:
People sought out Doctors in the past even when they actively hurt you and bled you
They did this because the doctor provided compassion and care that had the best intentions - they cared about their patient and the Art of Medicine
Physicians don’t act on business motives. They act on patient care motives.
You can see the #ArtofMedicine HashTag Social Media Statistics here and analytics here
Tuesday, March 18, 2014
Google Glass in Healthcare - Part 1 the Basic Facts
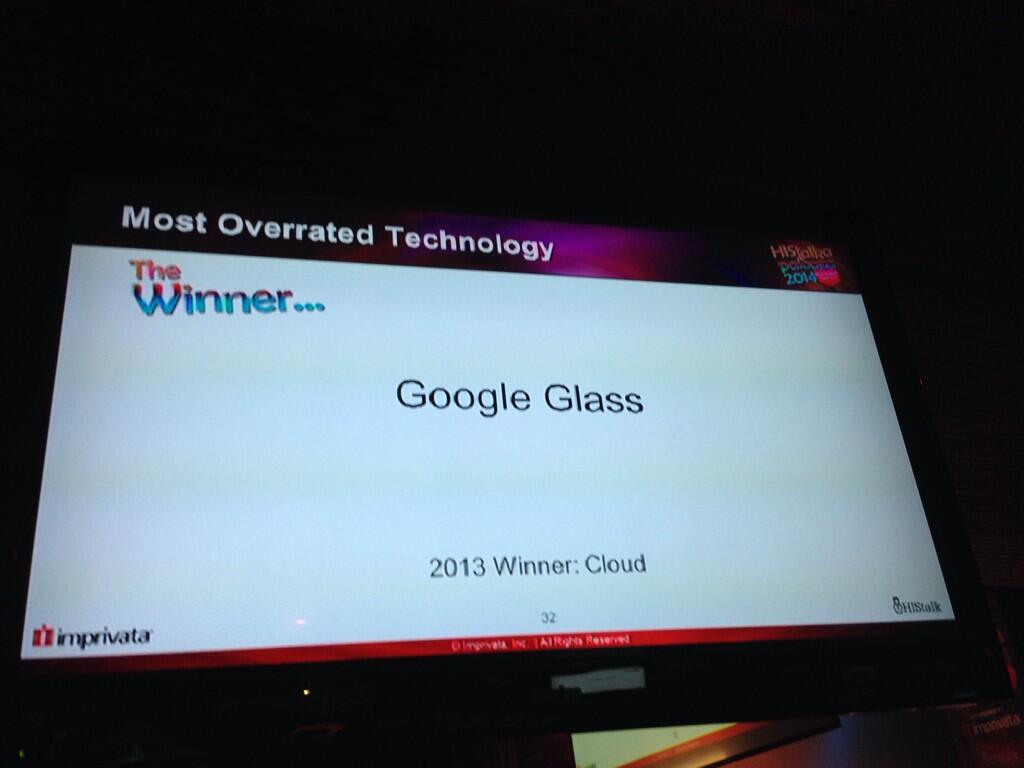
HIMSS was exciting and despite the HIS Talk HISies awarding Google Glass the most over rated technology:
I know I am biased as one of the lucky Google Glass Explorer as can be seen in this post from MedCity Watching for Wearables at #HIMSS14:
I think they are wrong and its not just Glass that will provide better more ready access to essential clinical data.
Not to say that the initial program like many launches have had their problems with early releases of technology not quite ready for prime time - remember the 1987 Apple Newton:
Even the omnipresent iPad struggled initially - most have probably forgotten the initial lukewarm reception of the iPad
had Apple talking about a price reduction.
Mat Honan (one on the same “Epic Hack”) wrote a piece about his early experiences “My Year with Google Glass” that highlighted some early acceptance challenges
and I would add Glass interrupts normal conversations and social behavior - but that is all now and like the mobile phone I believe it will be come a natural part of our technical fabric. Think back to 2007 and how pulling out a phone in a meeting was frowned upon - now it seems part of the fabric of many of the meetings I attend.
But it was Mat’s commentary on the impact it had on his perception fo phones that really stuck out for me
That’s not to say that Google Glass can solve this problem and in its current state and acceptance it might cause more challenges - but the potential is there to blend information access and capture into a physician patient interaction that remains all about the patient
Glass will provide improved access to essential clinical data to clinicians but as my friend Chuck Webster has pointed out on several occasions this is not just for clinicians. Patients are already accessing the internet in droves for clinical information, researching their conditions and that of their relatives and communities abound with resources and support for conditions from common to rare.
Before talking about some of the potential medical applications it is worth detailing the technology. Google Glass is basically a computer with 12Gb of memory attached to your head in the form of glasses. It has a heads up display with voice activation and has some apps that can be installed:
In its simplest form just transmitting images in real time can offer some advantages for diagnosis - in Rhode Island they are planning on implementing Google Glass for the ED doctors to obtain real time consults with dermatologists.
And this from Kareo showing a patient education application that records the physician patient interaction and then makes it available afterwards for additional review:
In this case featured in the ER doctors use Google Glass and QR codes to identify patients which featured Dr. John Halamka, CIO of Beth Israel Deaconess Medical Center which he talked about in his blog detailing their experience (oddly the article talking about this refers to text that appears to have been changed or taken down):
And this concept by the way was top of everyone's wish list that I talked to in my unofficial survey of engaged and interested observers of my own pair. I'll paraphrase
This recent piece on Healium featured in the Seattle King5 News Station: Seattle Doctor testing Google Glass for Surgery in the ER (click on the link if the video does not show below to see it in action)
Part 2 will cover medical applications and how Google Glass technology can be applied in a busy clinical setting
Oh, @wareflo - this could hurt... #HIStalkapalooza14 Most overrated tech @histalk HISSIES #HIMSS14 pic.twitter.com/dThovzVWvo
— Mandi Bishop (@MandiBPro) February 25, 2014
I know I am biased as one of the lucky Google Glass Explorer as can be seen in this post from MedCity Watching for Wearables at #HIMSS14:
I think they are wrong and its not just Glass that will provide better more ready access to essential clinical data.
Not to say that the initial program like many launches have had their problems with early releases of technology not quite ready for prime time - remember the 1987 Apple Newton:
Even the omnipresent iPad struggled initially - most have probably forgotten the initial lukewarm reception of the iPad
had Apple talking about a price reduction.
Mat Honan (one on the same “Epic Hack”) wrote a piece about his early experiences “My Year with Google Glass” that highlighted some early acceptance challenges
- Glass is socially awkward
- People get angry at Glass
- Wearing Glass separates you
and I would add Glass interrupts normal conversations and social behavior - but that is all now and like the mobile phone I believe it will be come a natural part of our technical fabric. Think back to 2007 and how pulling out a phone in a meeting was frowned upon - now it seems part of the fabric of many of the meetings I attend.
But it was Mat’s commentary on the impact it had on his perception fo phones that really stuck out for me
Glass kind of made me hate my phone — or any phone. It made me realize how much they have captured our attention. Phones separate us from our lives in all sorts of ways. Here we are together, looking at little screens, interacting (at best) with people who aren’t here. Looking at our hands instead of each other. Documenting instead of experiencing.Which resonates with me an the Art of Medicine campaign and the struggle clinicians have with focusing on the patient (To learn more, download the eGuide Art of Medicine in a digital world). As Dr. Edward C. Grendys, Jr. said in his article: There’s no room for technology in end-of-life care decisions:
From initial diagnosis through to surgical therapies, chemotherapy treatments and even end-of-life care, my job is to listen, assess and provide educated decisions that ultimately impact the health and wellness of another human being…. it’s my belief that when talking face-to-face with a patient about a care plan aimed at eradicating their body of a disease that threatens to take them away from their family, there’s no room for paper, computers and/or mobile devices. In these most intimate of conversations, the focus has always and must remain on the communication between the caregiver and the patient on the receiving end. That, in its purest essence, is what practicing the art of medicine is truly all about.
That’s not to say that Google Glass can solve this problem and in its current state and acceptance it might cause more challenges - but the potential is there to blend information access and capture into a physician patient interaction that remains all about the patient
Glass will provide improved access to essential clinical data to clinicians but as my friend Chuck Webster has pointed out on several occasions this is not just for clinicians. Patients are already accessing the internet in droves for clinical information, researching their conditions and that of their relatives and communities abound with resources and support for conditions from common to rare.
Before talking about some of the potential medical applications it is worth detailing the technology. Google Glass is basically a computer with 12Gb of memory attached to your head in the form of glasses. It has a heads up display with voice activation and has some apps that can be installed:
Facts
- Google Glass is basically a computer attached to a pair of glasses
- Google Glass has a display that is projected in front of the Right Eye that is a high resolution display equivalent of a 25 inch high definition screen from eight feet away
- Google Glass has a camera that points forward and can take pictures (5MP) or video (720p) that is closely aligned with the view you see from your own eyes
- Google Glass is voice activated using speech recognition to interact with the glass computer
- Google Glass works best when connected to the internet
- Google Glass Integrates with an Andorid Phone with a limited set of functions available for the iPhone
- Google Glass has no built in illumination so pictures or video taken in dark conditions do not work well
- The screen can be hard to see in bright light
Myths
- If someone is wearing Google Glass they are recording me
- False - The device is not set up to record continuously and will only record a video or photo based on an action by the wearer (either a spoken request
- OK Glass, take a picture
- or by pressing a button on the google glass device
- Once Someone Has recorded something on Google Glass it is Publicly Posted
- False - it requires an action on the part of the Glass owner to post the material to the internet otherwise it resides on the Google Glass device. It will be synchronized with the users Google+ account for automatic backup (much like photos are backed up from the iPhone to iCloud but like iCloud remain private to the user unless they elect to share them)
- Google Glass is constantly capturing data and transmitting it to the Internet
- False. Without an internet connection Google Glass simply stores any recorded information in the glass memory. And unless you have set it to record there is no data being captured
- Google Glass tracks users and unsuspecting bystanders
- False - Google Glass is not tracking or recording anything unless instructed to do so by the user
- Video sharing and storage: Physicians could record medical visits and store them for future reference or share the footage with other doctors.
- A diagnostic reference: If Glass is integrated with an electronic medical record (EMR), it could provide a real-time feed of the patient’s vital signs.
- A textbook alternative: Rather than referring to a medical textbook, physicians can perform a search on the fly with their Google Glass.
- Emergency room/war zone care: As storied venture capitalist Marc Andreessen proposed in a recent interview, consider ”dealing with wounded patients and right there in their field of vision, if they’re trying to do any kind of procedure, they’ll have step-by-step instructions walking them through it.” In a trauma situation, doctors need to keep their hands free.
- Helping medical students learn: As suggested by one blogger, a surgeon might live stream a live — and potentially rare — surgery to residents and students.
- Preventing medical errors: With an electronic medical record integration, a nurse can scan the medication to confirm whether it’s the correct drug dose and right patient
In its simplest form just transmitting images in real time can offer some advantages for diagnosis - in Rhode Island they are planning on implementing Google Glass for the ED doctors to obtain real time consults with dermatologists.
And this from Kareo showing a patient education application that records the physician patient interaction and then makes it available afterwards for additional review:
In this case featured in the ER doctors use Google Glass and QR codes to identify patients which featured Dr. John Halamka, CIO of Beth Israel Deaconess Medical Center which he talked about in his blog detailing their experience (oddly the article talking about this refers to text that appears to have been changed or taken down):
When a clinician walks into an emergency department room, he or she looks at [a] bar code (a QR or Quick Response code) placed on the wall. Google Glass immediately recognizes the room and then the ED Dashboard sends information about the patient in that room to the glasses, appearing in the clinician’s field of vision. The clinician can speak with the patient, examine the patient, and perform procedures while seeing problems, vital signs, lab results and other data.
And this concept by the way was top of everyone's wish list that I talked to in my unofficial survey of engaged and interested observers of my own pair. I'll paraphrase
If I could get it to recognize someone and provide me with their name when I meet them that would be fantastic!But it is in urgent care where there is so much potential:
This recent piece on Healium featured in the Seattle King5 News Station: Seattle Doctor testing Google Glass for Surgery in the ER (click on the link if the video does not show below to see it in action)
"If I want to look at for example radiology I can double tap ‘radiology...There's his chest x-ray, it just popped up, oh he's got a middle lobe pneumonia"
Part 2 will cover medical applications and how Google Glass technology can be applied in a busy clinical setting
Subscribe to:
Posts (Atom)